With CGM and FGM systems becoming the norm to manage type 1 diabetes, it can be hard to imagine what we ever did without them. At-home glucometers weren’t available until the 1970s. Knowing what we know now, it’s kind of scary to think of how people measured glucose levels before that. One of the most common ways to test glucose levels was to use Benedict’s Solution or another similar urine analysis method.
This post contains affiliate links
What is Benedict’s Solution?
At-home glucometers weren’t commercially available until 1978. Up until that point, glucometers were only available in doctors’ offices to be used by doctors.
Even when they became available to patients, it was difficult to get one. They were expensive and bulky. They were not nearly as accurate or easy to use as the glucometers we know and use today.
So, lots of people continued with their old method of diabetes management. Boiling their urine to test for glucose.
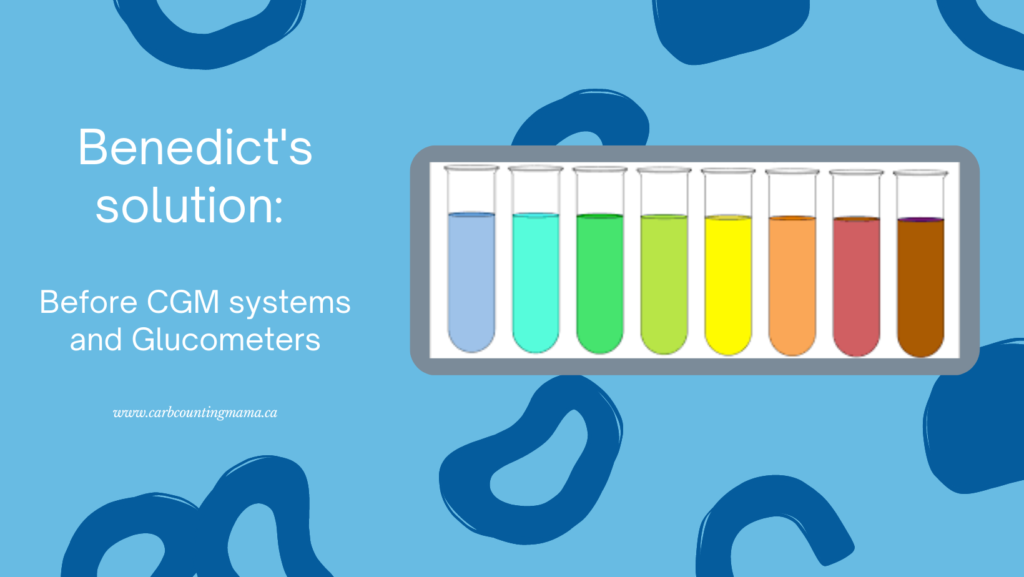
Benedict’s Solution (also sometimes called Benedict’s Test or Benedict’s Reagent) was one of the main products that diabetes patients used to determine their glucose levels. It is a chemical mixture that can identify glucose in a urine sample.
It’s a mix of copper sulfate pentahydrate, sodium carbonate, and sodium citrate. The solution itself is a deep blue color.
I’ll spare you the chemistry lesson, but basically, these chemicals will change the solution to green, yellow, or even a deep red color if glucose is added and the mixture is heated.
How to use Benedict’s Solution
The instructions for Benedict’s Solution were fairly straightforward:
- Put 40 drops of Benedict’s Solution in a test tube
- Add a few drops of urine to the test tube
- Stand the test tube in boiling water for 3-5 minutes
- Observe for color changes in the solution
If the solution stayed blue, that meant there wasn’t any glucose in the urine. But if it changed to green, yellow, or red, that meant increasing levels of glucose. Red indicated very concentrated glucose in the urine sample.
Then what?
Between 1936 and 1982, people used a very slow-acting animal insulin. It was made from pigs or cows. In general, you were told not to eat sugar and you had to take one injection of insulin per day.
Often, people would test their urine in the morning and then take their insulin. That insulin amount would vary depending on the color of your urine sample that day.
If you’ve been at this T1D thing for a while…
You may have noticed several problems with this method.
Of course, it was the best option at the time. There was no other way to test your glucose levels at home and there were no synthetic insulins in existence.
However, the way things were done back then was really dangerous for many people. Here are a few reasons:
1. The “sugar diabetes”
Diabetes was often referred to as “the sugars” or “the sugar diabetes”. People knew that there was a connection with sugar, but knowledge and education about diabetes were severely lacking.
Most people were told to “stop eating sugar”. They were only supposed to eat sugar if their glucose was low. Now, that’s all well and good, but most people didn’t understand that that meant more than the sugar that we use in the kitchen to bake yummy treats.
People were often eating baked goods (with sugar substitutes of course), fruit, milk, etc. with no knowledge that it was affecting their glucose levels. People who were strict with their no-sugar diets were often consuming hundreds of grams of carbs on a daily basis and had no idea.
Nowadays, we count carbs, not sugar. We know that carbohydrates (and even certain amounts of protein and fat) convert in our systems to simple sugars. And we calculate insulin doses based on all of it, not just strictly “sugar”.
It’s very possible that this is why so many people have misconceptions about T1D and sugar nowadays. If you think about it, it wasn’t that long ago that it was true. People with diabetes weren’t supposed to eat sugar. That was true well into the 1980s.
2. Testing urine to determine the glucose level
There are some problems with testing urine for things like this. We have the same problems today with urine ketone meters vs blood ketone meters.
- Urine isn’t current. The glucose that is in your bladder is not the same as the glucose that is in your bloodstream. The stuff in your bladder is your body trying its best to expel excess glucose. And, since urine can build up in your bladder over several hours, it’s telling you what was in your system several hours ago rather than at the time of testing.
- It’s a chemistry experiment. Whether or not you understand science and chemistry, these tests can give false results fairly easily due to user error. Too much or too little solution or too much or too little urine could cause the color to come out differently than it should. And let’s not forget the fact that if you got distracted while doing this test and it boiled for too long, you’d explode a test tube all over your kitchen.
- Dosing based on this urine sample. Yes, the insulin used back then was very slow acting, so it wasn’t going to drop your glucose level quickly. But, since the urine sample could be inaccurate for various reasons, it was basically like throwing a dart at a dartboard and hoping for the best.
3. What is low glucose?
As I mentioned, people were told to eat sugar if they were low. But, if they were only testing their urine once a day, and blue was a good color that didn’t necessarily mean your glucose was low, how did people know when they were low?
This is a really scary part of T1D care before at-home glucometers. You may have guessed it already. The only way you would be able to tell if you’re having a low is if you’re hypo-aware (meaning you know how your body feels when your blood glucose goes too low) or… you start shaking, have a seizure, or lose consciousness.
There was no testing for lows. No finger pokes. No glancing at your phone to see your current glucose trend. All you could do was rely on symptoms. And as we know, many people are hypo-unaware and don’t start exhibiting physical symptoms until they’re quite low.
It’s important to know about things like Benedict’s Solution
To know what people used to have to do to manage their diabetes. Understanding that these things were the standard methods until only a few decades ago.
The first thing I asked when my son was diagnosed with T1D 10 years ago was, “Is it going to shorten his life?” And the doctors told me that it wouldn’t.
Statistics do show a slightly shorter life expectancy for people with T1D. And it’s so important to remember that people who used these methods are included in those statistics. That, while they were doing the best that they could at the time, our technology and knowledge of T1D have improved so much over the last few decades.
During many of our lifetimes, T1D management has gone from boiling your urine on the stovetop and hoping for the best, to being able to glance at a number on your phone, TV, or car dashboard that tells you what your or your child’s glucose level is. In current time. And we have technology that calculates the insulin dose for us, allows us to bolus remotely, and some insulin pumps that will adjust the insulin amount without user input when it sees bg going up or down.
All in the span of about 4 decades. Can you imagine what will happen over the next 4 decades?
~ Leah
If you’d like to read some real-life stories about growing up with T1D before all of this technology, I highly recommend checking out Richard Vaughn’s “Beating the Odds: 64 Years of Diabetes Health”
For more tips and stories about T1D, join the Carb Counting Mama email list, and make sure to head over to the Carb Counting Mama Facebook page and “like” it.
Leave a Reply